
Because the white blood cells originally came from her body, there was no risk of her immune system attacking the cells. Once the functioning adenosine deaminase gene had been inserted into white blood cells by the virus, these white blood cells were injected back into Ashanthi’s blood. In this case, the vector was a virus that had been modified so it no longer caused disease. Vectors are ‘vehicles’ used by scientists to insert new genes into DNA. Once outside of the body, new, working copies of the adenosine deaminase gene were inserted in to the cells via a vector. The process of gene therapy to treat Ashanthi’s condition involved getting some of Ashanthi’s white blood cells from her blood. the alternative treatments are expensive and/or hazardous.the target cells for the therapy are lymphocytes (white blood cells), which are accessible, easy to grow and easy to put back into the body of a patient.the adenosine deaminase gene is very small and easy to manipulate in the laboratory.adenosine deaminase levels vary widely in the normal population so tight control of the introduced gene is not important.the disease results from the loss of function of a single gene.
Gene therapy for scid trial#
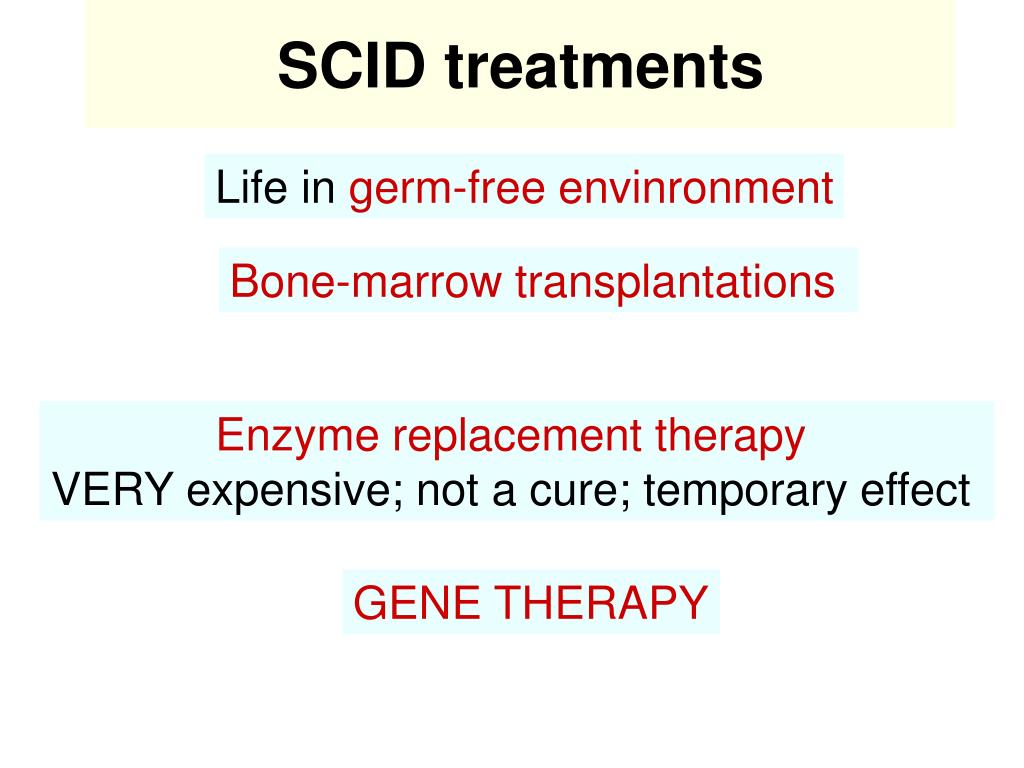
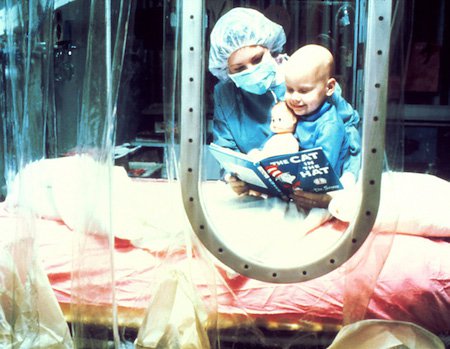
In the early 1990s, while Ashanthi’s parents were desperately searching for another option for their child, permission to perform the first gene therapy trial on humans was being obtained. For this reason, children with SCID were often known as ‘bubble babies’. Unfortunately however, this option was ruled out due to the lack of compatible bone marrow donors.Īt that time, if neither of these treatments were possible, the only way affected children could survive was by total isolation in an artificial, germ-free environment. In the case of Ashanthi, a transplanted bone marrow would increase white blood cell production and give her an effective immune system with the ability to fight infection. It produces red blood cells, platelets and white blood cells. Bone marrow is a spongy tissue found in the centre of our bones. The second treatment option was a bone marrow transplant from a compatible donor. By the age of four however, her health began to deteriorate and another option was needed.Īt that time the only way SCID-affected children could survive was by total isolation in an artificial, germ-free environment. Initially, she responded well and developed some resistance to infections. The first was regular injections with the adenosine deaminase enzyme (ADA-PEG), which Ashanthi started receiving from the age of two. Antimicrobial drugs can be used to treat these infections in individuals with SCID but they only provide short-term benefits.īefore the advent of gene therapy, there were only two ways to treat Ashanthi’s SCID. It left her vulnerable to even the mildest of infections, resulting in symptoms such as recurrent ear or chest infections, and persistent thrush in the mouth or throat. This deficiency prevented her body from producing the white blood cells that are required to fight infections. In Ashanthi’s case, the disease was caused by the absence of the enzyme adenosine deaminase (ADA). The patient was a four year old girl called Ashanthi who was suffering from a very rare disease known as severe combined immunodeficiency (SCID). The first ever gene therapy trial was initiated in 1990 by Dr William French Anderson. Gene therapy is a medical technique, first developed in 1972, that uses genes to treat or prevent disease.


 0 kommentar(er)
0 kommentar(er)
